Did that title pull you in? Good! That was my plan! At this point, I am sure most of you have at least heard of the term “Fecal Microbiota Transplant” (FMT) or “Fecal Transplant.” It is currently being studied as a potential treatment for IBD patients so I want to do a series of blog posts on Fecal Microbiota Transplant so you can be up to date on this current research topic. It sounds gross I know, but it is a really amazing treatment in specific situations. I want to talk to you about FMT, what it is, why it is important and could it possibly be used as a treatment for IBD patients?
What is Fecal Microbiota Transplant?
A fecal transplant is what it sounds like, transplanting fecal matter from one person (healthy person) into another person (sick person). It has actually been used for quite some time now for certain GI infections. This treatment is usually a last resort treatement, meaning it is only used when other conventional treatments have failed. What happens first is finding a donor, and this is not easy. The potential donor needs to go through some rigorous testing because when you are transplanting fecal matter you have to be extremely careful to make sure you don’t give someone another type of infection. They test the donor for all kinds of illnesses and diseases. Like, have they been on antibiotics recently? Do they smoke, drink alcohol? They examine every little thing they can to make sure this will be a safe procedure. There was a study that came out that said you have a better chance of getting into Harvard Medical School than being an FMT donor, basically, it’s very hard to find a good donor. Once the donor is cleared they then collect the stool sample. After this is completed they prep the sample that will be given to the patient. Before they transplant the stool the patient receiving the sample will do bowel prep, just like you would if you were getting a colonoscopy. They do this to “lavage” the bowels which will help get rid of some of the bacteria that are in the GI tract. Now, how do you the patient get the prepped fecal sample into your GI tract? There are a couple of ways this can be done. They can do a colonoscopy and use the scope to put the feces in the colon, you can do the Nasoduodenal tube, this is a tube from the nose to the dueodenum (small bowel). There is some work going into putting this in pill form so yes, “poop pills.” Lastly you can do an FMT enema. Sounds great right? Why would something so gross sounding be done?
Why is FMT used?
FMT is used to treat patients who have recurrent Clostridium difficile (C.diff) infection or Clostridiumdifficile colitis who have not responded to standard therapy. What is Clostridium difficile infection you ask? Well, Clostridium difficile is a bacterium that is part of the natural gut flora, meaning we all have it in our guts and usually we get along with it just fine. Our guts are home to trillions of bacteria and in a normal gut, you have a balance of beneficial bacteria and bacteria that can potentially cause illness, which we call “opportunistic pathogens.” These opportunistic pathogens are kept under control by the beneficial bacteria and we all live happy together. It is all about the balance of beneficial bacteria to opportunistic bacteria. They also provide nutrients for us like Vitamin K and they also eat our waste which aids in this protection from pathogenic species. If you want to know more about the gut microbiome check out the posts I did detailing everything you need to know about the gut microbiome ☞Gut Microbiome the Basics and ☞Gut Dysbiosis and Disease. What happens is when a patient takes antibiotics say for a sinus infection the antibiotics don’t just kill off the bacteria that are causing the infection, they also kill off our beneficial (good) bacteria. When there are not enough beneficial bacteria in our guts, the bacteria that have the potential to cause disease or infection do exactly that. Cause infection. C. diff infection is a potentially life-threatening infection if left untreated. It causes horrible GI problems such as diarrhea, nausea, vomiting, extreme abdominal pain, etc. The ironic thing is that to cure the infection you use another antibiotic usually Flagyl and if that doesn’t work Vancomycin, and if that doesn’t work then you are probably looking at the Fecal Microbiota Transplant. It has a really good success rate in clearing the infection when standard antibiotic treatment was not enough. Remember earlier I said that when you take antibiotics you don’t just kill off the bacteria causing the infection but you also kill off the beneficial bacteria? What FMT does is restore this balance of bacteria and can get the C. diff infection under control. Once again you can refer to the links above if you would like to learn more about the Gut Microbiome, Dysbiosis and how that is involved in diseases. Now, what about FMT as a treatment for IBD?
FMT and IBD.
Generally speaking IBD patients compared to the normal population have what is called gut dysbiosis. This means that IBD patients have an unbalanced amount of bacteria in their guts which has been shown to be important. The basis of FMT is restoring the balance of bacteria in the gut right? So if IBD patients have this dysbiosis and we know it is contributing to disease wouldn’t it make sense to try and use FMT as a potential treatment? I think so. And so do others which are why it is being investigated! Conclusion.
My next FMT post will be about a cool FMT study involving UC patients who were non-responsive to traditional therapies and pretty much at their last resort. I won’t give anything away, but it has some pretty exciting results! I will talk a little more about FMT and IBD in this next post. I definitely do not want to over “hype” this because it still needs a lot of research, but it is promising. Once again you can check out my previous posts on the gut microbiome and how that relates to diseases in the links I provided above. I hope you will continue on this FMT journey with me as we dive into it a bit more and see what the research is showing us.
![]()
References:
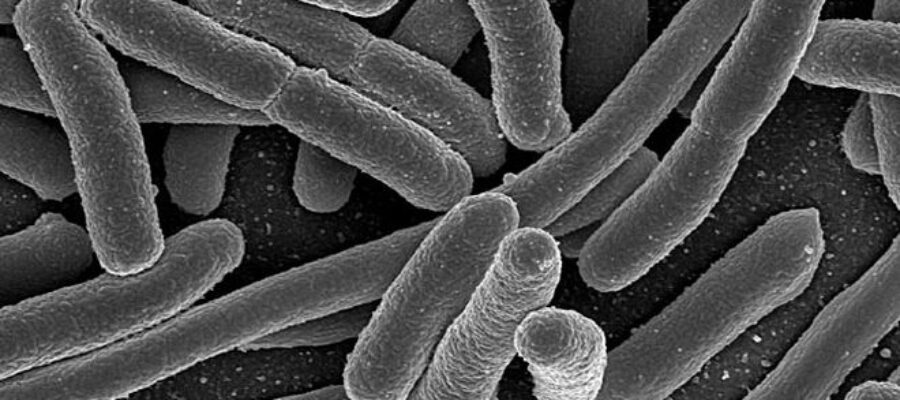
Image: Scanning Electron Microscopy of E. coli
Image Credit: National Institutes of Health (NIH)
http://www.hopkinsmedicine.org/gastroenterology_hepatology/clinical_services/advanced_endoscopy/fecal_transplantation.html
http://www.openbiome.org/about-fmt/
Sartor, R. B., & Mazmanian, S. K. (2012). Intestinal Microbes in Inflammatory Bowel Diseases. The American Journal of Gastroenterology Supplements, 1(1), 15–21. http://doi.org/10.1038/ajgsup.2012.4
Buttó, L. F., & Haller, D. (2016). Title: Dysbiosis in intestinal inflammation: Cause or consequence Dysbiosis in intestinal inflammation: cause or consequence 1. International Journal of Medical Microbiology. http://doi.org/10.1016/j.ijmm.2016.02.010